Content
Module 3: The Patient
Introduction
This module covers the decision-making process and preparation of the patient requiring an awake intubation. The choice of oral vs. nasal intubation is discussed.
Who needs an awake intubation?
The hardest part of performing an awake intubation, is deciding if the patient requires one. Although it is common to equate 'awake intubation' with bronchoscopic intubation, this is not necessarily the case. The first decision relates to consciousness/muscle relaxation; the second decision relates to the device chosen.
Airway Approach Algorithm (W.H. Rosenblatt): Use this interactive tool to decide if an awake intubation is necessary. View the airway approach algorithm.
- Must the airway be controlled?
- Yes No
- Could laryngoscopy be (at all) difficult?
- Yes No
- Could supralaryngeal ventilation be used (if needed)?
- Yes No
- Is the stomach empty?
- Yes No
- Will the patient tolerate an apneic period?
- Yes No
- Awake Intubation or spontaneous ventilation
- Intubation after induction
- Consider regional/infiltrative
Which patients are best suited for awake bronchoscopic intubation?
This procedure is best for patients for whom there is time to adequately anesthetize with topical agents (however, several techniques allow rapid local anesthesia). The patient should be co-operative and able to understand the planned procedure.
Which patients are poorly suited for an awake intubation?
Patients should not undergo awake intubation if there is:
- a language or developmental barrier to co-operation
- hypoxia requiring immediate intubation
- risk of airway bleeding including coagulopathy or friable tissues (bronchoscopy can make bleeding worse)
- blood or significant sections in the airway (can make the view impossible)
- a patient with narrowed airways will have further reduction in effective lumen for gas exchange as the bronchoscope is advanced
Patient preparation and consent
Consent
Explain to patient why they require an awake intubation – establishing rapport and co-operation is an important part of the process. For example:
"An important part of my job is to look after your breathing during the operation. Under a general anesthetic you will not be breathing on your own – instead we will be placing a breathing tube into your windpipe and using a ventilator to help you. Your anatomy differs from normal, such that it is likely to be difficult to place the breathing tube. Therefore we need to do this before you go to sleep, and once we have confirmed that the breathing tube is in the correct location, we can safely give you the anesthetic. We will give you sedation and freezing medication which will make this as comfortable as possible and you may have little or no memory of this later. We will proceed at a pace you are comfortable with and we can stop at any time. Please raise your hand during the procedure if you are uncomfortable and need me to stop."
Physical preparation
- IV
- Monitors: pulse oximetry, ECG and BP
- Oxygen: nasal prongs, oxygen catheter into opposite nostril or via the working channel of the bronchoscope
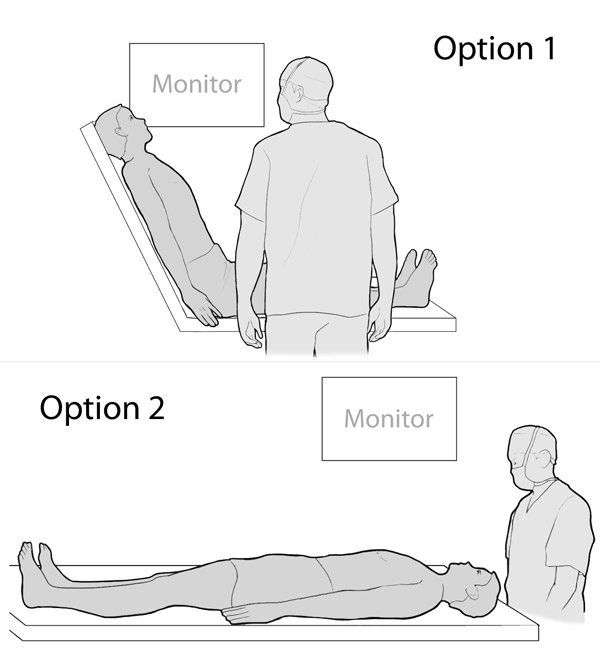
Patient positioning
Option 1: Patient sitting at least 45° upright, facing the operator, monitor on the patient's left
Option 2: Patient supine with the operator in the normal intubating position, monitor on the patient's right
Continue to: Module 3: Advanced Knowledge

