VIRTUAL Patient
Rationale for Virtual Patients
Teaching clinical expertise and the cognitive processes involved in clinical reasoning that physicians use to arrive at a diagnosis has been a challenge since medicine began to be taught as a discipline. There seems to be a growing consensus that at least one important aspect of diagnostic acumen is pattern recognition. The development of pattern recognition requires exposure to a large number of cases. However, there are increasingly limited opportunities for students to get this exposure, and the experience they get is restricted to what happens to turn up in their clinical rotations.
Supplementing these clinical experiences with simulated clinical cases, or “virtual patients” provides the opportunity for exposing students to a wider variety and a greater number of cases than they would otherwise encounter. Virtual patients can also demonstrate different ways that the same disease can be manifested, and even deliberately creating the conditions that often result in diagnostic error. Feedback on the student’s performance provided by the program will improve their skill in applying their knowledge to the solution of diagnostic problems.
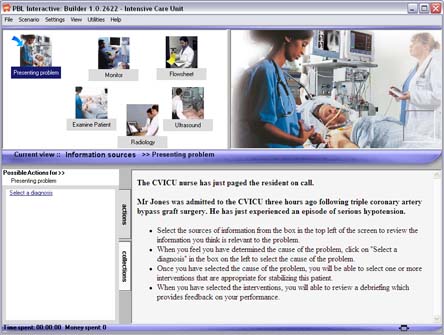
PBLI - A tool for creating virtual patients
 Problem Based Learning Interactive (PBLi) is a software tool developed at the University of Queensland for creating diagnostic problems of all kinds. Although initially intended for simulating agricultural problems, we have adapted it to create diagnostic problems in medicine. This involves the initial development of a template of a normal person, then inserting abnormal values in the template to create each new diagnostic problem.
Problem Based Learning Interactive (PBLi) is a software tool developed at the University of Queensland for creating diagnostic problems of all kinds. Although initially intended for simulating agricultural problems, we have adapted it to create diagnostic problems in medicine. This involves the initial development of a template of a normal person, then inserting abnormal values in the template to create each new diagnostic problem.
Virtual patients created with PBLI have the following features
- The student can gather information about the patient in any order they decide based on the initial presenting complaint. Students can:
- Select appropriate questions to elicit the history of the presenting illness, the past medical history, the family history and psychosocial history.
- Carry out a functional assessment of relevant body systems
- Carry out a physical assessment of the patient.
- Order any necessary laboratory tests or diagnostic imaging.
- Consult with other specialists.
- The software tracks the student’s progress in gathering information, and provides a time and cost for each action the student takes.
- The student then makes a diagnostic decision, selecting the appropriate choice from a list of potential plausible diagnoses, and receives feedback on their choice.
- A debriefing is then presented to the student, providing feedback on errors of commission (gathering irrelevant information) and omission (missing important information).
- Optionally, the student’s path taken in solving the case and the debriefing can be E-mailed to an instructor. This allows the case to be used for student evaluation or research in clinical reasoning.