Content
Spinal Ultrasound
Click on an item to jump to that section.
- Introduction
- Longitudinal paramedian approach
- Transverse approach
- Step-by-step assessment of the typical lumbar spine
- Atypical sonograms
- Ultrasound: a promising technical advance in spinal and epidural techniques
- References
Introduction
The practice of epidurals and spinals in Obstetrics relies on the palpation of anatomical landmarks that are not always easy to feel. A good assessment of the spine includes a careful examination to determine if the vertebrae are aligned, and to locate the iliac crests, the lumbar spinous processes and the interspaces. These are the landmarks required to perform a safe lumbar puncture, because they identify the level of the spine at which the puncture should be performed and the optimal puncture site. Other important aspects of the technique such as the angle of puncture and the distance from the skin to the ligamentum flavum cannot be assessed based on inspection and palpation. If a patient is overweight or has scoliosis, or even worse, is overweight and scoliotic, the appropriate assessment of the lumbar spine becomes even more challenging, increasing changes of failures and complications of the spinal or epidural anesthesia placement.
Complications of spinal and epidural anesthesia include patient discomfort, trauma to various structures such as nerves, vessels, ligaments and bones, and accidental dural punctures with subsequent postdural puncture headaches. In the past, these complications have been minimized or avoided by meticulous assessment of the landmarks, optimal positioning of the patient and refinement of the technique. Now, with the availability of bedside ultrasound, we can "see" more of the anatomical structures and our technique has become much less blind. Perhaps it is appropriate to say that the "art" is giving way to the technology.
Ultrasound has recently been utilized to facilitate lumbar spinals and epidurals. Spinal ultrasound is especially challenging, because the structures we need to image are protected by a very complex, articulated encasement of bones, which affords very limited acoustic windows for the ultrasound beam. In addition, the structures we want to visualize are located even deeper than we are accustomed to when we use ultrasound for peripheral nerve blocks or central lines. For these reasons, the ultrasound probe used for spinals and epidurals must be a low frequency, curved probe (2-5 mHz). The low frequency ultrasound beam penetrates deeper, but loses in image resolution. There are two acoustic windows that are effective for lumbar spine sonographic assessment: one seen on the transverse approach, and the other seen on the longitudinal paramedian approach. The information from each of these two scanning planes supplements the other.
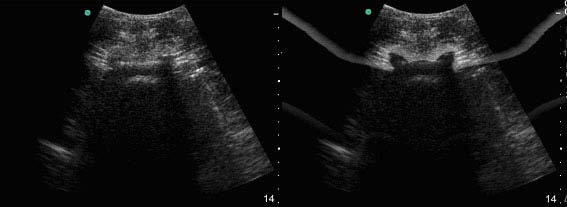
Figure 1. Left: Typical sonogram of an interspace in the transverse plane. Right: Artistic enhancement to facilitate memorization of the pattern (flying bat).
Compared to ultrasound for peripheral nerve blocks where a number of different sonographic patterns have to be memorized, spinal ultrasound is simpler in the sense that only two patterns have to be memorized: one for the transverse approach, and the other for the longitudinal approach (midline or paramedian). For the transverse approach, the typical view is that of a flying bat (Figure 1); for the longitudinal approach, that of a saw (Figure 2).
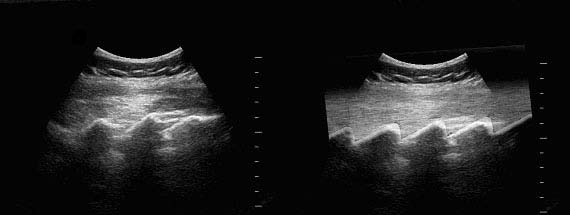
Figure 2. Left: Typical sonogram of the sacrum and multiple interspaces in the longitudinal plane. Right: Artistic enhancement of the "saw" pattern.
Longitudinal paramedian approach
The structures that will be identified by the ultrasound include the sacrum, multiple lamina, multiple interspaces containing the ligamentum flavum/posterior dura mater and the vertebral body/posterior longitudinal ligament/anterior dura mater, the CSF and the spinal canal. The acoustic window provided by the longitudinal plane is superior to that provided by the transverse plane, such that one can often see the ligamentum flavum and the posterior dura as distinct structures (Figure 3).
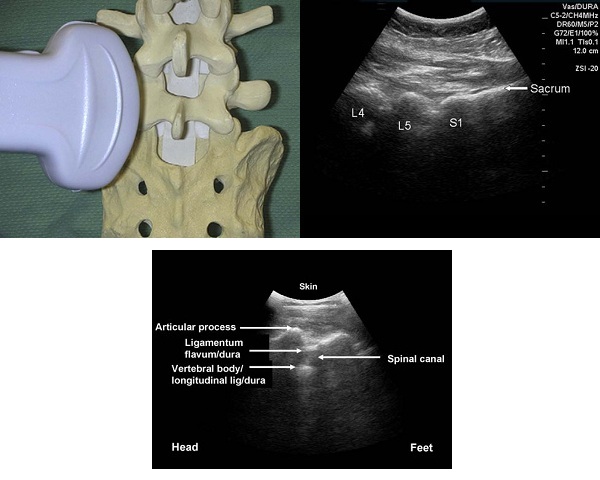
Figure 3. Top left: probe is positioned in the longitudinal paramedian plane. Top right: sacrum is seen as a continuous hyperechoic line parallel to the skin, approximately 5 cm deep continuing as "cracks" (interspaces) alternating with "lumps" (lamina of different vertebrae). Bottom: close up at a lumbar "crack" (interspace), with lamina of two different vertebrae on the right (caudad) and on the left (cephalad). The elements of the interspace can be easily identified, including distinct images of the posterior dura mater, the epidural space and the ligamentum flavum. The vertebral body-posterior longitudinal ligament-anterior dura mater is seen as a single unit.
Transverse approach
The structures that will be identified by the ultrasound include the spinous process (Figure 4), the articular processes, the transverse processes, the vertebral body, the ligamentum flavum, the posterior longitudinal ligament, and the anterior and posterior dura mater (Figure 5). Typically, with the current resolution of our equipments, the ligamentum flavum and the posterior dura are seen as a single structure, similar to the anterior dura, the posterior longitudinal ligament and the vertebral body.
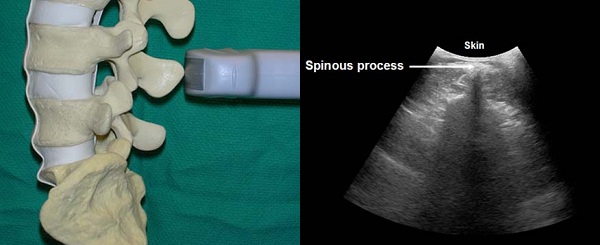
Figure 4. Typical sonogram of the spinous process in the transverse plane. The spinous process is seen as a hyperechoic signal close to the skin (in slim patients), continuing as a vertical acoustic shadow, sometimes triangular in shape.
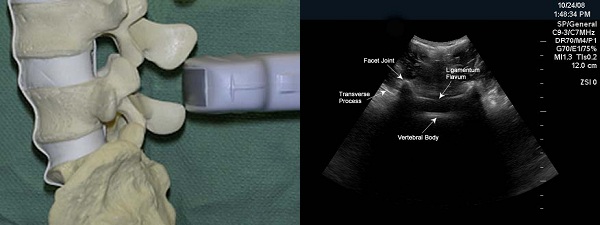
Figure 5. Typical sonogram of an interspace in the transverse plane, showing very symmetric images of transverse and articular processes on each side, in addition to the ligamentum flavum-posterior dura mater and the vertebral body-posterior longitudinal ligament-anterior dura mater.
Step-by-step assessment of the typical lumbar spine
The patient should be positioned similar to the positioning for the actual placement of an epidural. It is suggested that novices learn with the patient sitting first. The scanning is performed initially in the left paramedian longitudinal plane. With the top of the buttock crease as a starting point, the ultrasound probe is moved in a cephalad direction in the left paramedian longitudinal plane in order to identify the upper end of the sacrum (L5-S1 interspace), and to determine the level of each lumbar interspace above. When a given interspace is aligned with the center of the screen (as if there were a virtual vertical line at the center of the screen crossing the "interspace"), the midpoint of the probe is marked on the skin. The clinician can mark one targeted interspace, or also has the luxury of marking all five lumbar interspaces.
Once the intervertebral levels are marked on the skin with a regular pen, the ideal insertion point for each interspace can be determined. This is done by switching the probe to the transverse plane. The insertion point is the intersection of the midline and the interspace. The midline is identified in the transverse plane by visualizing the spinous process, which is seen as a small hyperechoic signal beneath the skin, continuing as a long, vertical, somewhat "triangular" hypoechoic shadow. With the image centered on the screen, a dot is marked on the skin at the midpoint of the probe. The probe is then slowly moved in a caudal or cephalad direction, to capture the best acoustic window of an interspace, including the ligamentum flavum, the dorsal dura mater, the ventral dura mater, the posterior longitudinal ligament, and the vertebral body, as well as the articular and the transverse processes. Once the best possible image of the interspace is captured, the transducer is held stationary and the image is frozen. The skin is then marked at the midpoint of the width of the probe -- this point represents the interspace. By connecting a vertical line intersecting the midline point, and a horizontal line intersecting the interspace point, the ideal insertion point is determined (Figure 6). The skin-LF distance, i.e., the depth to the epidural space is measured with the aid of a built-in caliper (Figure 7).
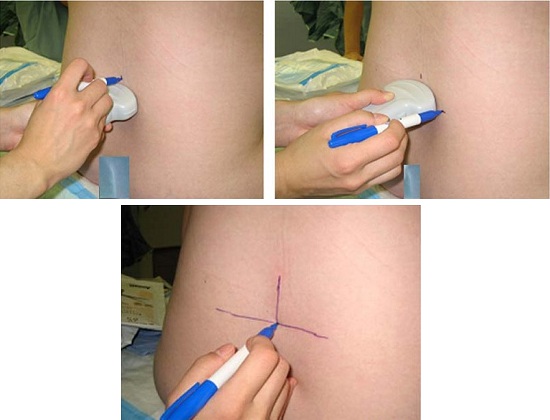
Figure 6. The insertion point can be easily and accurately determined in the transverse plane. The midline and the interspace are determined as outlined, and points are marked on the skin as illustrated. Horizontal and vertical lines are drawn intersecting these points; the intersection of the lines determines the insertion point.
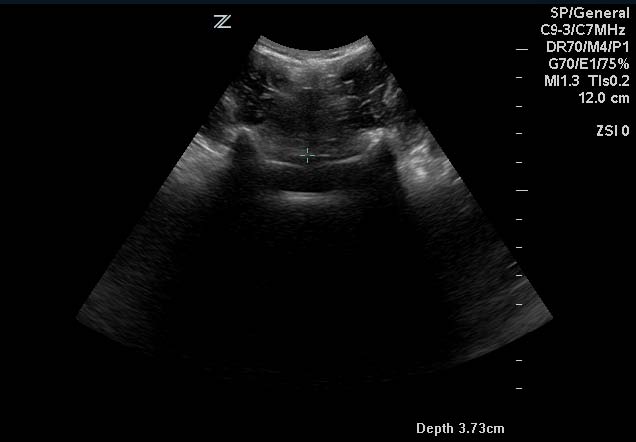
Figure 7. The distance to the ligamentum flavum is determined with the aid of a built-in caliper. If the sonogram of the ligamentum flavum is not clear enough in the transverse plane, it is advisable to double check the distance to the same structure in the longitudinal plane. The distance from the skin to the ligamentum flavum in the longitudinal plane is usually a few millimeters shorter than in the transverse plane, but clinically they can be used interchangeably.
Atypical sonograms
Ultrasound of the lumbar spine is also useful to identify atypical anatomy, including that associated with obesity, and scoliosis. The scoliotic spine does not present the mirror image of the articular and transverse processes on each side, as typically seen in the transverse plane. The spinous process often no longer appears as a vertical shadow but rather projects as an oblique line to one of the sides. The articular processes are sometimes located at different distances from the skin. And finally, the ligamentum flavum may be only partially visible. All these anomalies confirm the presence of asymmetry at the level of a given interspace (Figure 8).
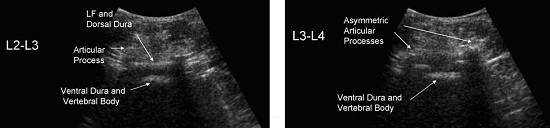
Figure 7. Left: typical sonogram of an interspace in the transverse plane. Right: atypical sonogram of an interspace, in the same patient, showing the asymmetric structures of scoliosis.
Ultrasound: a promising technical advance in spinal and epidural techniques
Bedside ultrasound can be extremely useful to facilitate spinal and epidural anesthesia placement by providing the following information:
- the exact interspace at which the puncture should be performed, which is especially important in spinals,
- the best interspace,
- the ideal insertion point,
- the angle of the puncture,
- the distance from the skin to the epidural space, and
- anatomical abnormalities, such as scoliosis.
Ultrasound provides both proven and yet to be proven advantages by:
- Providing a superior teaching tool for spinals and epidurals, as it facilitates the learning curve, and may increase safety during the learning curve,
- shortening the duration of procedures,
- increasing the comfort of procedures,
- decreasing the number of attempts and the associated trauma,
- possibly decreasing the number of accidental dural punctures,
- forecasting difficult epidurals (similar to difficult intubations),
- transforming difficult epidurals into easy epidurals, and
- helping in the selection of the best equipment for the spinal/epidural.
References
- Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Efficacy of ultrasound imaging in obstetric epidural anesthesia. J Clin Anesth 2002; 14:169-75.
- Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Ultrasound imaging facilitated localization of the epidural space during combined spinal and epidural anesthesia. Reg Anesth Pain Med 2001; 26: 64-7.
- Grau T, Leipold RW, Conradi R, Martin E, Motsch J. Paramedian access to the epidural space: The optimum window for ultrasound imaging. J Clin Anesth 2001; 13: 213-17.
- Arzola C, Davies S, Rofaeel A, Carvalho JCA. Ultrasound using the transverse approach to the lumbar spine provides reliable landmarks for labor epidurals. Anesth Analg 2007; 104:1188-92.
- Carvalho JCA. Ultrasound-facilitated epidurals and spinals in obstetrics. Anesthesiol Clin 2008; 26(1): 145-158.
- Lee Y, Tanaka M, Carvalho JCA. Sonoanatomy of the lumbar spine in patients with previous inadvertent dural punctures during labor analgesia. Reg Anesth Pain Med 2008; 33: 266-270.
- Balki M, Lee Y, Halpern S, Carvalho JCA. Ultrasound imaging of the lumbar spine in the transverse plane: correlation between estimated and actual depth to the epidural space in obese parturients. Anesth Analg 2009; 108:1876-81
- Borges B, Wieczorek P, Balki M, Carvalho JCA. Sonoanatomy of the lumbar spine of pregnant women at term. Reg Anesth Pain Med 2009; 34:581-85

